Education
Critical concepts regarding POCUS peripheral vein cannulation should be well known for our medical professionals, aiding in improving cannulation success and catheter dwell time and avoiding complications. We are providing links and resources to help you understand the importance of POCUS.


Onsite Education
ScAn Pro Inc. offers onsite education and workshops for individuals or small groups wishing to learn the basics of POCUS
Online Education
Nearly 30% of all patients who visit the ER in the US each year will require venous access. Bedside ultrasound-guided peripheral IVs (USGPIV) offer an alternative to central venous cannulation and external jugular cannulation for patients in which PIV access cannot be obtained, thereby reducing the risks of infection and the need for additional resources that are associated with the aforementioned procedures. * The prevalence of difficult venous access in complex patients is 59.3%. Significant risk factors include being female and a history of complications related to vascular access.**
Do You Know This!
How Many People Visit ER per year in the US?
In 2020
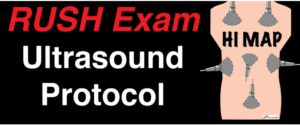
In a recently published update, the American College of Emergency Physicians identified 5 main areas of POCUS scope of practice in the emergency department setting. These include both cardiac and non-cardiac POCUS applications. The five areas include resuscitation, diagnosis, procedural guidance, signs/symptom evaluation, and therapeutic or monitoring indications.
POCUS for Vascular Access and Venipuncture
The New England Journal of Medicine
Ultrasound-Guided Peripheral IV Placement
Overview
Placement of peripheral intravenous (IV) catheters is a fundamental skill that all health care professionals should possess. Unfortunately, it can be difficult to obtain IV access in some patients, including obese patients, children, and patients who have undergone placement of many IVs or who have a history of difficult IV access. Ultrasound guidance enables visualization of veins that are not apparent on physical examination, resulting in fewer needlesticks, more rapid cannulation, and less discomfort in patients with difficult IV access.1-3 Ultrasound-guided IV placement is indicated when it is difficult or impossible to use traditional techniques. There is no contraindication to ultrasound-guided IV placement, but it is unnecessary when traditional techniques are sufficient. Health care providers who are proficient in standard placement techniques will find it relatively easy to learn ultrasound-guided techniques.
Ultrasound guidance facilitates placement of peripheral IV catheters when standard techniques fail. Learning ultrasound-guided techniques is relatively easy, especially for providers who are proficient in the placement of standard IV catheters. Small linear transducers and long IV catheters are ideal for ultrasound-guided IV catheter placement.
“The New England Journal of Medicine”
Click on the picture for the video
Other Related Article Links
POCUS in the Emergency Setting
POCUS in the Critical Care Setting
Basic RV assessment
POCUS in the Office and Clinic
Ultrasound screening during wellness visits spots abnormalities in 94% of patients.*